Inflammaging: What is it and how can you prevent it
Inflammaging refers to low-grade, sterile, chronic inflammation that increases with age and can contribute to health declines, age-related diseases, and frailty.
The exact causes are still unclear, but one theory called “garb-aging” suggests that damaged molecules accumulate in cells, triggering inflammation through immune signaling. While this may play a role in inflammation, it’s probably not the only cause. The aging of the immune system might also contribute to inflammaging, but there’s still a lot to learn about how immunosenescence (the aging of immune cells) drives this inflammation. Overall, inflammaging involves a complex relationship between cell senescence, immunosenescence, and inflammation, which affects health in later life.[ref]
Importantly, inflammaging may be a cause of aging and the diseases of aging.
Often overlooked but vitally important is that inflammation has a counter pathway, the resolution of inflammation. And the resolution of inflammation could be the key to health in aging, the key to stopping inflammaging.
The resolution of inflammation is an active process
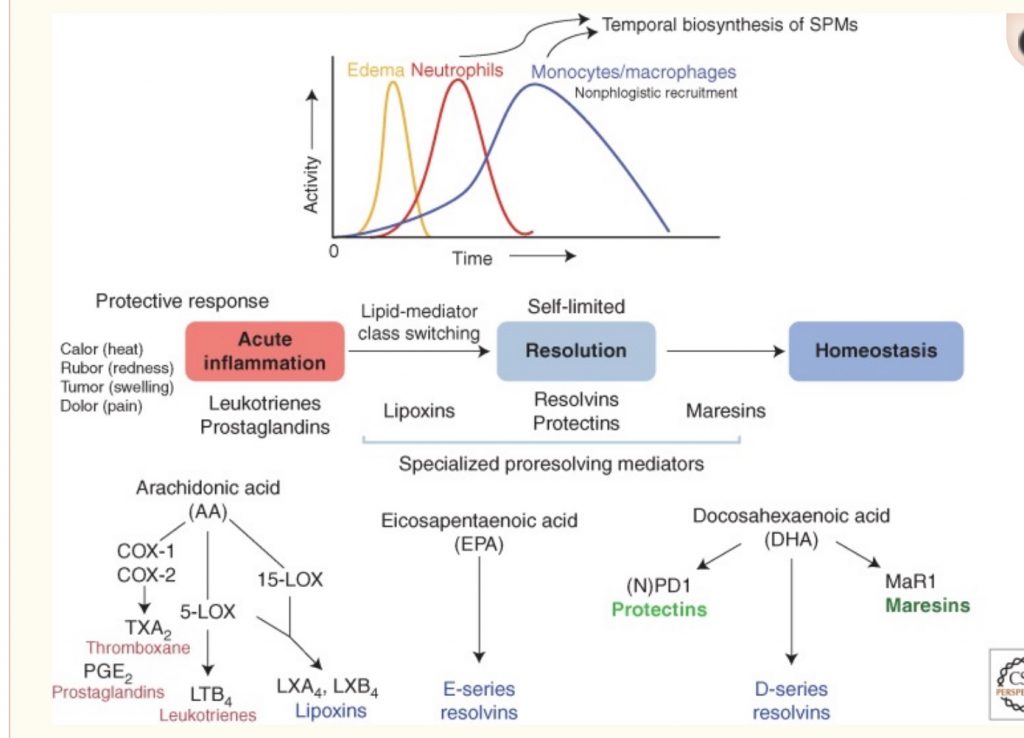
Inflammation is a complex process with multiple pathways and cytokines involved in recruiting immune system cells to an area of inflammation.
Inflammation doesn’t just go away.
The resolution of inflammation is an active process that goes on at the same time as the inflammatory cascade of events.
Lipid mediators derived from omega-3 fatty acids are at the heart of the resolution of inflammation. DHA and EPA are the building blocks for specialized pro-resolving mediators (SPMs). And these pro-resolving mediators actively work to decrease inflammation and promote a return to homeostasis.[ref]
The role of specialized pro-resolving mediators in healthy aging: A treatment for inflammation
Animal studies show that pro-inflammatory eicosanoids, like prostaglandin E2, are produced at the same levels in both old and young animals. But the older animals failed to produce the pro-resolving lipid mediators at the same level as young animals. Specifically, lipoxin A4, resolvin D6, protectin D1, and maresin 1 were lacking in aging muscles, which was associated with greater inflammation and impaired regeneration. Injections of resolvin D1 partially reversed the inflammation in aged muscles. The authors conclude that “aging results in deficient local biosynthesis of specialized pro‐resolving mediators in muscle and that immunoresolvents may be attractive novel therapeutics for the treatment of muscular injuries and associated pain in the elderly, due to positive effects on recovery of muscle function without the negative side effects on tissue regeneration of non‐steroidal anti‐inflammatory drugs.”[ref]
What did all that mean? In a nutshell, old muscles produce plenty of inflammation, but they don’t produce enough pro-resolving mediators. Thus, inflammation wins in aged muscles, which can’t repair and be restored like young muscles.[ref]
In aging, chronically elevated proinflammatory cytokines can include IL-6 and TNF-alpha. A recent study looked at the impact of DHA and EPA separately on levels of inflammatory cytokines. While there was some overlap, the specific pro-resolving mediators created from EPA lowered TNF-alpha levels, whereas DHA reduced both IL-6, TNF-alpha, and MCP1 levels.[ref] Additionally, NF-kB is inhibited by SPMs.[ref]
In women with osteoporosis and osteopenia, maresin I levels were decreased in compared to women of the same age with healthy bone density. Inflammation is thought to be a factor in the breakdown of bone mass in osteoporosis, and the researchers theorized that lower maresin 1 levels allowed chronic inflammation to continue to decrease bone mass.[ref][ref]
Neurodegenerative disorders and SPMs:
Neuroinflammation, or inflammation in the brain and nervous system, is a hallmark of aging. The activation of microglia – immune system neurons – occurs in and may be the cause of Alzheimer’s and Parkinson’s diseases. Activated microglia produce inflammatory cytokines including TNF-alpha, IL-1B, and more. Even outside the scope of Alzhemer’s, chronically activated microglia and neuroinflammation can cause the loss of cognitive function.[ref]
Stopping the chronic inflammation in the brain may help prevent neurodegenerative disorders. Post-mortem studies on Alzheimer’s brains showed decreased SPM levels, compared to age-matched controls without neurodegenerative diseases. Numerous animal studies and cell-line studies show that SPMs (specifically resolvins and maresins) are essential for resolving neuroinflammation.[ref]
Animal models of Alzheimer’s clearly show benefits for reducing inflammation in the brain by using specific pro-resolving mediators.[ref]
Human trials on DHA and EPA for Alzheimer’s have largely shown little benefit. However, almost all of the trials used 1g or less per day of DHA/EPA. A clinical trial using over 2g of DHA showed significant changes in brain DHA and EPA levels in Alzheimer’s patients.[ref]
Perhaps a specific SPM is needed? Resolvin D1, which is derived from DHA, along with vitamin D (active form 1,25-D3) was shown to increase clearance of amyloid-beta by macrophages. “In all AD macrophages, phagocytosis was increased by 1,25D3 and RvD1 in a concentration-dependent and additive fashion”.[ref]
SPMs and Immune Response to Viruses and Bacteria:
Your immune system protects you from viral and bacterial infections, of course. But as we age, the immune response can become imbalanced. An overactive immune response, such as seen in Covid or sepsis, can kill you.
Specialized pro-resolving mediators directly impact pathogen infections.
The flu virus is less active when SPM levels are higher, and certain strains of flu have been shown to use up lipoxin, and the reduction then allows the virus to spread. Protectin D1 is an SPM derived from DHA. It is also important in regulating the inflammatory response to influenza. Treating mice infected with the flu virus with supplemental protectin D1 increases survival.[ref]
Studies also show that SPMs help with modulating immune response as well as reducing viral replication in herpes simplex virus and RSV infections.[ref]
Macrophages are a type of white blood cell. They come in two flavors – M1, which increases inflammatory signaling, and M2, which modulates and regulates inflammation. The cytokine storm that caused severe Covid and death is based in a switch to M1 macrophages in the lungs along with secondary bacterial infections. SPMs help to facilitate the clearance of cellular debris, such as in infected lung tissue. Additionally, SPMs push macrophages towards the anti-inflammatory M2 type.[ref]
How much DHA and EPA do you need?
A study in Alzheimer’s patients used 1.7 g DHA and 0.6g of EPA daily. The researchers found that dosage of DHA/EPA could prevent the cognitive declines and the dropping levels of SPMs seen in the placebo arm. The 1.7g of DHA and 0.6 g of EPA was enough to maintain cognition in people with mild Alzheimer’s, but didn’t reverse it.[ref]
Inhibiting COX1 and COX-2 with NSAIDs generally delays the formation of pro-resolving mediators. Low-dose aspirin, though, is an exception. Asprin modifies COX-2 in a way that blocks inflammatory prostaglandins but still triggers the formation of resolvins and lipoxins. Specifically, aspirin at 75mg increases the formation of lipoxin A4.[ref]
Other aspirin-triggered SPMs include AT-lipoxin A4, AT-resolvin D1, and AT-resolvin D3.[ref][ref] Aspirin-triggered SPMs are unique in that they have a prolonged half-life and act to resolve inflammation for longer.[ref]
Clinical trials on SPMs and the diseases of aging:
A clinical trial investigated SPMs in fat tissue from people who were obese vs normal weight. The fat tissue from obese people had greater inflammation and lower concentrations of SPMs. Additionally, in the obese adipose tissue, the genes involved in converting DHA and EPA into SPMs were downregulated. The study participants took 3g/day of fish oil (1.1 g EPA, 0.8g DHA) or 3 g/day of corn oil (placebo). The normal weight participants had a greater decrease in inflammation in their adipose tissue at the end of 12 weeks compared to the overweight group. The researchers speculated that the downregulation of genes involved in creating SPMs was limiting the effects in obesity.[ref] I would love to see this taken to the next level with either supplements SMPs (instead of DHA/EPA) or perhaps higher doses of fish oil.
Researchers tested to see what DHA alone would do in patients with rheumatoid arthritis. The double-blind crossover trial included 2.1g/day of DHA from microalgae compared to sunflower oil (placebo), each for 10 weeks. The daily use of 2.1g of DHA decreased swollen joins and ultrasound scores in the patients compared to their baseline. The DHA increased maresins and resolvins. [ref]
Another clinical trial looked at how SPMs increased in response to doses of EPA/DHA equivalent to eating fish 1, 2 or 4 times a week. The increase over 12 months was linear, with higher DHA/EPA consumption corresponding to higher SPMs.[ref]
In overweight women, 1.8g EPA+DHA per day decreased several inflammatory markers and increased SPMs.[ref]
A study using an SPM specific supplement found that it improved pain and quality of life after one month in people with chronic pain syndromes.[ref]
Not all trials of DHA and EPA showed positive results:
- In a trial of prescription DHA/EPA-carboxylic acid, the 3g prescription dosage did not prevent major cardiac events in people with statin-treated heart disease.[ref]
- A one month of 4g of DHA/EPA in people with peripheral artery disease did not show changes to flow-mediated dilation compared to placebo.[ref]
- A clinical trial of 4.4g/d of fish oil in patients with peripheral artery disease (PAD) looked at the increase in SPMs as well as other changes. While SPM levels increased significantly, there was no change in walking speed or flow-mediated vasodilation in the patients.[ref]
There are lots of questions surrounding clinical trials with fish oil (in my mind). The quality of fish oil likely matters a lot. Additionally, the timing of SPMs in the inflammatory cascade seems important. Perhaps EPA and DHA are better at preventing diseases of chronic inflammation rather than curing them after the damage has been done.
The study using vitamin D plus DHA/EPA brings up an interesting point – when you get DHA and EPA naturally in fish, it usually comes with vitamin A and D. Perhaps the combination is needed. Another publication points to supplements not bringing benefits due to “industrialized processing of marine oils due to the application of high heat, as well as treatments such as bleaching and winterizing.”[ref]
What about algae supplements that contain DHA and EPA? Marketed for vegans, algae is now being produced commercially as a source of DHA and EPA. Bioavailability studies on algae show that the DHA and EPA is absorbed similarly to fish oil or eating fish.[ref]
Eating fish instead of supplements?
Fish oil supplements come with questions around quality and oxidation. You don’t want contamination, and you also don’t want the oil to be oxidized or rancid. Quality matters a lot.
The Okinawan and Mediterranean diets are linked to longevity. Both diets feature eating fish and seafood along with vegetables.[ref]
So what if you just want to eat fish to meet your needs for DHA and EPA? Well, you need to keep in mind that some fish are contaminated with mercury. Mackerel, salmon, and hering are high in DHA/EPA. Lake trout are also a good source. Grab the fishing pole and head to the lake?[ref]
Other sources of DHA and EPA in the diet include grass-fed beef and egg yolks from chickens that are free range. (Free range eggs have about 3 times the omega-3 content compared to conventional eggs.)[ref][ref][ref]
Conclusion: Solving Inflammaging
Having sufficient DHA and EPA is vital for resolving inflammation and for healthy aging.
However, clinical trials on fish oil supplements for specific diseases are often underwhelming. To me, this paints a picture of needing DHA and EPA available constantly to prevent the damage from chronic inflammation, but adding DHA and EPA after years of damage may not be effective for reversing the condition (e.g. clogged, fibrotic arteries).
Our modern diet has shifted dramatically towards more omega 6 and less omega 3 fatty acids. This shift is likely one cause of the rise in so many chronic diseases.
Read more about specialized pro-resolving mediators and chronic inflammation here.
